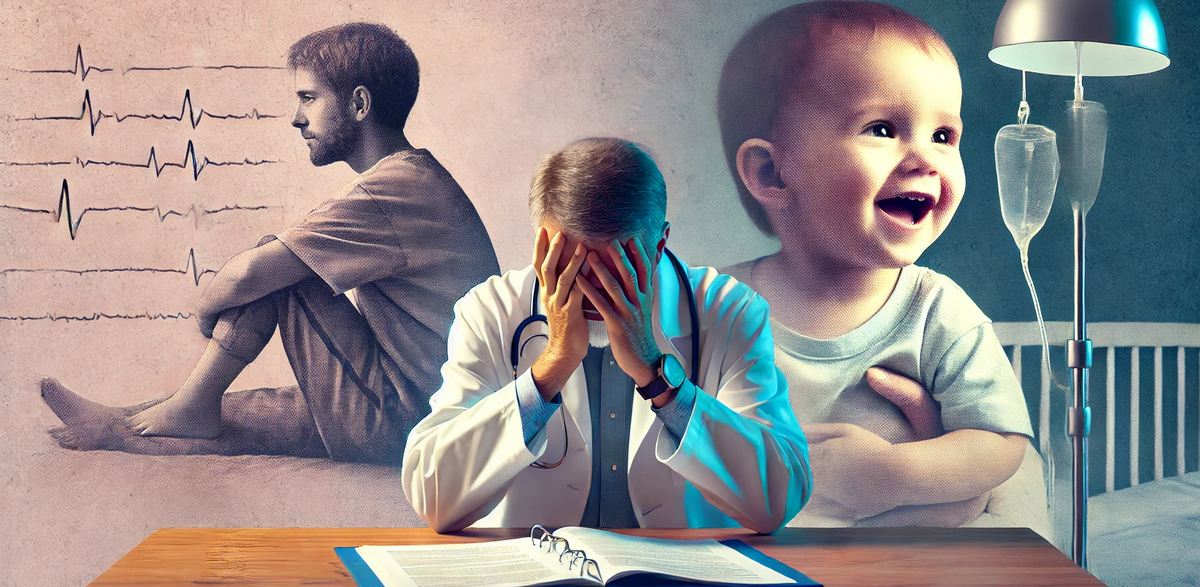
The medical principle of "do no harm" is central to healthcare ethics, emphasising the importance of patient well-being above all else. However, this principle is flipped on its head when doctors know they could alleviate suffering but are constrained by outdated guidelines and bureaucratic red tape.
This is the reality for many paediatricians treating children with intractable epilepsy. Medicinal cannabis has been shown to significantly reduce seizures and improve quality of life for patients who don’t respond to traditional treatments. Yet, rigid guidelines leave these doctors unable to act in their patients' best interests.

The Ethical and Financial Contradiction
For children with intractable epilepsy, the stakes couldn’t be higher. Without effective treatment, they face frequent, life-disrupting seizures that can lead to hospitalisations, developmental delays, and a diminished quality of life. Medicinal cannabis could break this cycle, but the current NHS system prioritises expensive hospital care over affordable, effective solutions.
Hospital Care Costs: £20,000 or more for a week of intensive care following a severe seizure episode.
Cannabis Medicines: Around £2,000 for a month’s supply, which could prevent seizures and enable home-based care.
Despite this disparity, NHS trusts often choose the costlier and less effective option, citing concerns over guidelines and liability.

Why Are Guidelines Lagging Behind?
Bureaucratic Barriers: NHS guidelines for medicinal cannabis remain overly restrictive, requiring lengthy specialist approvals.
Lack of Awareness: Many healthcare professionals are not adequately educated about the benefits of medicinal cannabis.
Stigma and Misconceptions: Cannabis still carries a stigma that influences decision-making, despite growing evidence of its medical value.

The Real Cost of Inaction
For families of children with intractable epilepsy, the impact is devastating:
Frequent Hospital Stays: Expensive, disruptive, and emotionally taxing.
Unnecessary Suffering: Children endure seizures that could be mitigated with timely access to cannabis medicines.
Financial Strain: Families often resort to private prescriptions which are unaffordable for many, and have to 'smuggle' medication through UK borders.

A Call for Change
The principle of “do no harm” must extend to the healthcare system itself. To truly prioritise patient well-being, the NHS must:
Simplify Access: Streamline the process for NHS prescribing medicinal cannabis to patients with intractable epilepsy.
Educate Healthcare Professionals: Equip doctors with the knowledge and confidence to recommend cannabis medicines responsibly.
Reform Guidelines: Update policies to reflect the growing body of evidence supporting cannabis as a treatment option.
Conclusion
When doctors are unable to prescribe effective treatments due to restrictive guidelines, the principle of “do no harm” is compromised. For paediatricians treating intractable epilepsy, medicinal cannabis represents a lifeline—one that could drastically improve outcomes and quality of life.
It’s time for the NHS to embrace evidence-based, compassionate care. Because when the tools to alleviate suffering exist, failing to use them doesn’t just “do harm”—it perpetuates it.
also read: This has just got to stop!
Published: 26/01/2025






You must be logged in as a member to add comments.
Become a member
Already a member? Log in or create an account.