
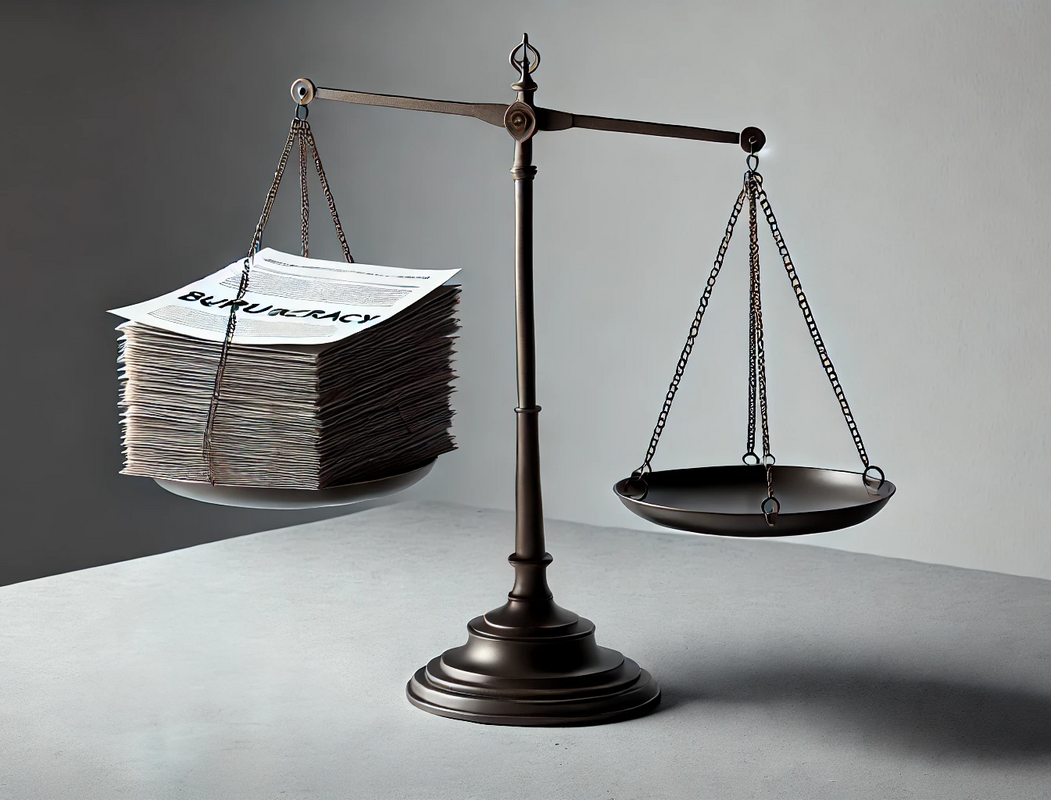
Despite the law change in 2018 allowing the prescribing of medicinal cannabis, and the compelling evidence of the effectiveness of cannabis-based medicines in managing seizures, many families are still battling excessive bureaucracy, financial barriers to accessing this life-changing treatments, and breaking the law to do so. These barriers not only cause unnecessary suffering but also highlight the irrationality of drug ‘safety’ committees such as NICE, that prioritise over-circumspection against the well-being of vulnerable individuals.
The BBC recently highlighted the significant challenges parents face in accessing medicinal cannabis for their children in the UK.
https://www.bbc.co.uk/sounds/play/m0026v6nw
It’s time for the U.K. Government to step in. Regulatory committees need to stop clinging to factless history and to embrace a more informed, pragmatic and compassionate approach to how individual patients process these naturally occurring plant medicines.
Understanding neurodiversity and chemical responses
Human responses to chemicals vary dramatically. For example, individuals who have ADHD/ADD who are prescribed substances like stimulants, which might cause hyperactivity in neurotypical individuals, but have the opposite effect—focusing the mind and providing a sense of calm. This paradoxical reaction is well-documented, particularly in the treatment of conditions like ADHD.
The psychotropic effect of THC on a patient with epilepsy may not have the perceived effect of being intoxicated as would a non-epileptic patient.
The failure of safety committees and regulators to allow the NHS doctors to freely prescribe medicinal cannabis, prevents epileptic children, and millions of others with chronic conditions, from accessing unlicensed special medicines that could enhance their quality of life.
The absurdity of current laws
Drug laws are riddled with inconsistencies, many of which are rooted in decades-old fears rather than modern science. Instead of focusing on harm reduction or the therapeutic potential of substances, regulators too often default to punitive approaches, demonising substances without fully assessing their context or benefits.
For example, caffeine is widely accepted despite its stimulant properties, yet other plant-based stimulants or psychoactive substances remain vilified. The law isn’t consistent; it’s arbitrary. This perpetuates harmful stereotypes and discourages the rigorous scientific research that could challenge these outdated narratives.

The danger of risk for risk’s sake
Blanket bans and scare tactics around substances often do more harm than good. Risk is an inherent part of life, but avoiding open dialogue about drugs and their effects doesn’t mitigate that risk—it magnifies it. By refusing to engage in honest discussions, regulators force individuals to navigate a dangerous black market rather than a regulated and safe system.
Moreover, banning substances because they could be “misused” ignores their potential benefits when used responsibly. Many pharmacological interventions, including life-saving medications, carry risks, but we don’t ban them outright—we regulate their use. Why should this approach not apply to other natural substances with therapeutic potential?
The case for pharmacognosy in everyday medicine
Pharmacognosy—the study of medicines derived from natural sources—has been side-lined in modern times by the need for cheaper synthetic, mass-produced patented medicines, yet it holds the key to numerous solutions for wellness and healthcare.
Nature has provided us with an incredible pharmacy of compounds, many of which are far less harmful and more effective than synthetic alternatives. By prioritising pharmacognosy, we can create a more balanced and holistic medical model, integrating traditional knowledge with scientific rigour.
However, to achieve this, regulatory committees must abandon stigma and promote research into the benefits of these substances. The continued criminalisation of cannabis, psilocybin, and other natural compounds is a glaring example of how stigma overrides science. These substances hold enormous potential, not just in medicine but in promoting wellness and improving lives.
The work of End Our Pain continues
End Our Pain is a UK-based advocacy group campaigning for better access to medicinal cannabis, especially for children with severe epilepsy. Since 2019, they have worked to raise awareness, lobby policymakers, and push for regulatory reforms to make cannabis-based medicines accessible and affordable for families in need.
Since 2019, the End Our Pain campaign has been tirelessly advocating for the needs of families, calling for observational trials to provide crucial evidence and support. This initiative gained even greater urgency during the COVID-19 pandemic, which magnified the struggles these families endure. Despite this progress, in June 2020, plans for observational trials were unexpectedly replaced by a second randomised controlled trial (RCT).
In 2021, End Our Pain escalated their efforts, delivering a heartfelt letter to the Health and Social Care Committee. Signed by 78 parents, the letter urged the government to address the critical need for access to medicinal cannabis.
By 2024, the campaign proposed a balanced approach: two observational trials—one to gather data from current medicinal cannabis users and another to support critically ill children in immediate need. This concept isn’t unprecedented. In 2013, the government granted early access to a cannabis-based medicine a year before formal trials began. One of the first recipients was a child given just six months to live. Thanks to this access, he is now thriving as an adult, with his data contributing to evidence later reviewed by NICE.
Looking ahead to 2025, End Our Pain remains optimistic. RCT trials are expected to commence, and the campaign is actively engaging with the National Institute for Health Research (NIHR) to move their proposed trials forward. They also hope to secure a meeting with Health Secretary Wes Streeting to ensure the needs of families remain a priority.
Learn more about the campaign’s efforts: https://cannabishealthnews.co.uk/2020/10/16/it-saved-zaks-life-but-were-not-out-of-the-woods-yet/
NICE and What Do They Do?
The National Institute for Health and Care Excellence (NICE) is an independent public body in the UK, dedicated to improving health and social care through evidence-based guidance and recommendations. NICE evaluates the safety, efficacy, and cost-effectiveness of treatments, ensuring that the NHS delivers consistent, high-quality care across the country. It provides clinical guidelines for healthcare professionals, helping them make informed decisions about patient care. NICE also advises on how NHS resources are spent, ensuring that treatments offer value for money while maximising their impact on public health.
NICE’s arguments against medicinal cannabis?
NICE’s concerns about medicinal cannabis largely stem from what they see as a lack of robust evidence to support its widespread use. They argue that high-quality clinical trial data, such as randomised controlled trials, is limited for many cannabis-based medicinal products. This is partly due to the legal and regulatory barriers that have historically restricted research in this area.
There is also hesitation about the potential long-term effects of medicinal cannabis, with concerns over dependency, cognitive impacts, and other side effects. NICE’s evaluations focus heavily on cost-effectiveness, and cannabis products are often perceived as expensive compared to the evidence of their benefits.
Although some conditions, such as epilepsy, multiple sclerosis, and chemotherapy-induced nausea, have shown positive responses to cannabis-based medicines, NICE remains unconvinced of its efficacy for broader applications like chronic pain. Furthermore, they stress that cannabis-based treatments should meet the same rigorous standards as any other medicine, cautioning against fast-tracking approvals without sufficient evidence.

Suggestions for NICE to enable NHS prescriptions of medicinal cannabis
To unlock the potential of medicinal cannabis within the NHS, NICE could adopt a more pragmatic and flexible approach. By expanding their evidence framework to include real-world data and patient-reported outcomes, they could address the unique challenges posed by cannabis’s limited research history. Looking at models from countries like Canada or Germany, where cannabis prescriptions are more common, could also help shape a balanced and effective strategy.
It is essential for NICE and the government to support investment in further large-scale clinical trials, particularly in areas where demand for medicinal cannabis is high, such as chronic pain or mental health conditions like PTSD. This research would fill the gaps in evidence and provide a stronger foundation for decision-making.
Patient-centred outcomes should also play a greater role in NICE’s evaluations. For many patients, medicinal cannabis offers significant improvements in quality of life, especially when conventional treatments have failed. Considering these benefits more seriously would better reflect the needs of those seeking relief through cannabis-based medicines.
The current cost-effectiveness model could be expanded to include indirect benefits, such as reduced opioid use, better mental health outcomes, and patients’ ability to return to daily activities or work. This broader view of value would better capture the wider societal benefits of medicinal cannabis.
Conditional approvals could provide a middle ground, allowing cannabis-based medicines to be prescribed on the NHS while collecting additional data to refine guidance. A specialised framework for evaluating cannabis medicines would also recognise their unique nature compared to traditional pharmaceuticals.
Collaboration is key. NICE could work more closely with the medical cannabis industry to ensure that guidelines reflect a balanced and inclusive perspective. Training for NHS clinicians on the use and benefits of medicinal cannabis would also empower them to make informed prescribing decisions, increasing both confidence and access.
By adopting these steps, NICE could help the NHS meet the needs of patients who are currently being left behind, without compromising their commitment to safety, efficacy, and value for money.
Time for change
The historic shame surrounding certain substances is no longer tenable. Policymakers must take bold steps to challenge outdated narratives, regulate sensibly, and embrace scientific research.
A system that criminalises individuals or denies them access to potentially life-changing treatments is not just unjust—it’s immoral.
We must prioritise compassion, evidence, and pragmatism in our approach to drug policy. It’s time to stop the harm caused by ignorance, fear and financial destitution, and to start valuing the incredible potential of the natural world in improving human health and wellbeing.
This has just got to stop! It’s time to normalise cannabis treatments for prescribers and patients.
Published: 26/01/2025







You must be logged in as a member to add comments.
Become a member
Already a member? Log in or create an account.